We Can’t Rly on Development of New Drugs Alone to Combat Antimicrobial Resistance
By the bioMérieux Editors | Reading time: 2 min 30s
Featured Expert: Chris Groke, PharmD, BCPS, BCIDP, Medical Science Liaison at bioMérieux
PUBLICATION DATE : OCTOBER 24 , 2022
Antimicrobial resistance (AMR) presents a global health crisis, as every day we encounter more infections that cannot be cured with existing antimicrobials. 2019 data shows that about 1.27 million deaths every year worldwide are directly attributable AMR, with an additional estimated 4.95 million deaths associated in some way to AMR.
At the same time, the majority of major drug companies have been scaling back or cutting antibiotic research due to development challenges. New antimicrobials may help improve patient treatment options and outcomes, especially against resistant infections, but the fight against AMR cannot rely on drug development alone.
Many pharmaceutical companies have been leaving the antibiotic business as a result of research obstacles and challenging business incentives that can prove too difficult to maintain for many companies. No new classes of antibiotics have been discovered since the 1980s. New antimicrobials can take 10 to 15 years and over $1 billion USD to bring to the market. If and when new antimicrobial drugs are discovered, they will need to be used wisely as the last line of treatment against highly resistant infections. According to the WHO, the clinical pipeline and the recently approved antibacterial agents are insufficient to tackle the increasing spread of AMR.
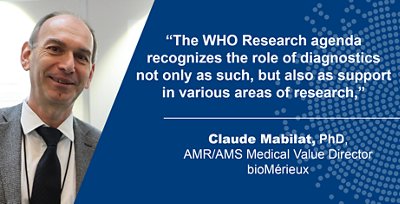
For Claude Mabilat, AMR/AMS Medical Value Director at bioMérieux, the importance given to diagnosis in this publication is a very pleasant surprise. “The WHO Research Agenda recognizes the role of diagnostics not only as such, but also as support in various areas of research,” he notes.
That focus is perhaps linked to the COVID-19 pandemic, which led to a sudden awareness of diagnostics’ important role in combating the spread of pathogens. From the perspective of health authorities, healthcare systems, and manufacturers, the role of diagnostics has become increasingly evident in the fight against antibiotic resistance as well.
“By highlighting diagnosis and defining a common language and shared orientations, this report will help the dialog with external partners, while serving as a catalyst for the activities in which we are already engaged,” underlines Mabilat.
How can we help preserve the efficacy of our antimicrobials?
Identification and surveillance can help maintain the effectiveness of our antimicrobials. As our diagnostic tools become more advanced, we can more accurately identify the cause of infections. Diagnostic tools can improve the speed and accuracy of a patient’s diagnosis, improving appropriate antibiotic selection and reducing the risk of side effects such as Clostridium difficile infections.
Diagnostic tools can also detect when resistance spreads and support public health tracking to identify threats and infection trends. By combining efficient diagnostics with data from resistance surveillance, we can more accurately treat infections with the correct antimicrobials from the beginning.
Health professionals can be stewards and do their part to help preserve the efficacy of antimicrobials by supporting the “five rights” of medication administration: right drug, right patient, right dose, right route, and right time. Staying informed on current outbreaks through the use of advanced analytics is another key component of a successful stewardship strategy.
While antibiotic development has slowed, AMR has not. We must work to preserve the efficacy of our antimicrobials through diagnostics and stewardship.
“This is an ongoing and actionable process,” says Groke. “Through diagnostic advancements coupled with data analytics, we can avoid potentially harmful and wasteful treatment.”
Opinions expressed in this article are not necessarily those of bioMérieux..
SHARE THIS:
- AMR AMS
< SWIPE FOR MORE ARTICLES >